The Administration for a Healthy America
Congressional Justification and legislative update
The Administration for a Healthy America (AHA) is a major initiative of the Trump administration and a core undertaking of HHS Secretary Kennedy, and yet few people know about this new, unified agency whose aim is to improve the health and well-being of all Americans.
The AHA represents one of the most sweeping reorganizations within the Department of Health and Human Services (HHS) since its formation, essentially merging programs that were scattered across multiple operating divisions (OPDIVs) into a single agency focused on public health, prevention, environmental health, and the health workforce.
The Congressional Justification is a formal budget document that each U.S. federal department or agency submits to Congress every fiscal year. Below is a link to the HHS AHA Congresional justification, which rolls in at 393 pages.
A close reading of the FY 2026 AHA Congressional Justification (CJ) shows the major recurring themes are:
Program consolidation and efficiency (“reducing duplication,” “streamlining operations”)
Prevention and primary care
Data-driven performance and accountability
Health workforce strengthening
Rural and underserved populations
Summary of the key points from the Administration for a Healthy America (AHA) FY 2026 Congressional Justification (CJ) document from U.S. Department of Health & Human Services (HHS):
Overview & Purpose
The AHA is a newly proposed operating division within HHS. Its mission is to “improve the health and well-being of all Americans” by consolidating and coordinating chronic disease prevention, health promotion, environmental health, mental/behavioral health, and other public-health oriented programs.
The FY 2026 budget request for AHA is $20.6 billion total, with approximately $14.1 billion in discretionary funds and $6.5 billion in mandatory and other sources.
The request aligns with the broader “Make America Healthy Again” initiative, emphasizing access to primary care, prevention, environmental health, mental/behavioral health, underserved and rural communities, and workforce development.
Major Program Areas
Here are some of the major programmatic areas. FY 2026 funding can be found in both the summary of the CJ and the CJ itself (linked above).
Primary Care & Access
Primary care programs.
Within that, the Health Center Program gets ~$6.1 billion to support roughly 1,400 health centers across more than 15,000 sites, serving low-income and underserved populations.
Other priorities: telehealth expansion, organ transplantation system modernization, and rural health programs (e.g., rural maternity/obstetrics, opioid response).
Environmental Health
Environmental health programs are grouped under AHA.
Within this are safe drinking water initiatives, childhood lead poisoning prevention, occupational safety and health, the National Institute of Environmental Health Sciences (NIEHS) research, the World Trade Center Health Program for 9/11 responders/survivors.
HIV/AIDS
Maternal & Child Health
The maternal & child health program
-- Key programs:The Maternal & Child Health Block Grant, Improving Maternal Health programs (including for maternal mental health hotline, screening/treatment of perinatal depression/substance use).
Pediatric Mental Health Care Access Grants.
Home Visiting Program.
Mental & Behavioral Health
Total for mental & behavioral health programs:
Major components:
Mental health.
Substance use prevention.
Substance use treatment.
Behavioral Health Innovation Block Grant.
Native American behavioral health & SUD resources.
Health Workforce
Key details:
National Health Service Corps (NHSC).
Teaching Health Center Graduate Medical Education.
Nursing workforce.
Behavioral health workforce development.
Policy, Research & Oversight
Performance & Strategy
AHA emphasizes a shift toward prevention (rather than solely treatment), addressing root causes of chronic diseases, and ensuring equity in underserved, rural, and tribal communities.
It also commits to data-driven decision-making, transparency, measurable outcomes, and streamlining/coordination of formerly separate programs.
Performance measures are aligned to national health objectives and outcomes rather than just outputs.
Proposed Program Eliminations / Streamlining
The budget document proposes to eliminate 23 programs under the “Primary Health” account.
It likewise proposes elimination of 9 programs under the Environmental Health account.
Under the Mental Health account, 40 programs are proposed for elimination.
Under the Health Workforce account, 14 programs are proposed for elimination.
These eliminations are designed to redirect resources toward the priorities of AHA, reduce duplication, and concentrate on fewer, bigger initiatives.
Key Takeaways & Implications
This is a major reorganization and consolidation within HHS – combining programs from OASH, HRSA, SAMHSA, NIEHS, and parts of the Centers for Disease Control and Prevention (CDC) into a single agency (AHA) to create efficiencies and clearer focus.
The emphasis is on prevention and reaching underserved populations, particularly in rural and tribal contexts.
The scale of funding is significant (~$20.6 billion request) and signals that the administration views public health, environmental health, behavioral health, and health workforce strengthening as interconnected priorities.
The restructuring suggests changes in how federal programs are delivered and funded, possibly shifting from many smaller targeted programs toward fewer, larger block grants with more flexibility (notably the Behavioral Health Innovation Block Grant).
For stakeholders (states, local health departments, community-based organizations, health centers), this means potential shifts in funding instruments, reporting/metrics, and eligibility/focus of programs.
Tracking performance and outcomes will be critical, the document highlights accountability, data-driven policy, and measurable impact.
Congressional Justification (CJ).
A Congressional Justification is a formal budget document that each U.S. federal department or agency submits to Congress every fiscal year. It explains:
What funding the agency is requesting (by program, line item, and account)
Why the funds are needed (policy rationale and expected outcomes)
How the funds will be used (staffing, grants, contracts, etc.)
How this year’s request compares to prior years’ appropriations
So, the “FY 2026 AHA CJ” means:
Fiscal Year 2026 Administration for a Healthy America Congressional Justification.
It’s the detailed supporting document that accompanies the President’s Budget submission to Congress, specifically for this new HHS operating division (the Administration for a Healthy America).
Primary Authoring Entity
The FY 2026 AHA CJ was written and submitted by the U.S. Department of Health and Human Services (HHS), specifically under the Office of the Secretary, which oversees all HHS operating divisions.
Because the AHA (Administration for a Healthy America) is a newly proposed operating division (OPDIV), the CJ was prepared by HHS budget and policy staff within:
The Office of Budget (OB) inside the Assistant Secretary for Financial Resources (ASFR)
In coordination with the Office of the Secretary (OS) and the AHA transition planning team
This means the document is not an external white paper or independent report; it’s an official HHS budget justification, authored internally by career and political budget officers and approved by HHS leadership.
Formal Submission and Approval
All CJs, including this one, follow a standard process:
Drafted by the agency’s budget staff (in this case, HHS/ASFR/OB working with AHA program offices).
Cleared through the HHS Secretary’s office (for policy alignment).
Reviewed by the Office of Management and Budget (OMB) within the Executive Office of the President.
Submitted to Congress alongside the President’s Budget for that fiscal year.
So the “authors” are not individual named people — it’s an institutional authorship, formally representing the Secretary of Health and Human Services.
The CJ is an executive-branch budget justification written for Congress, by HHS.
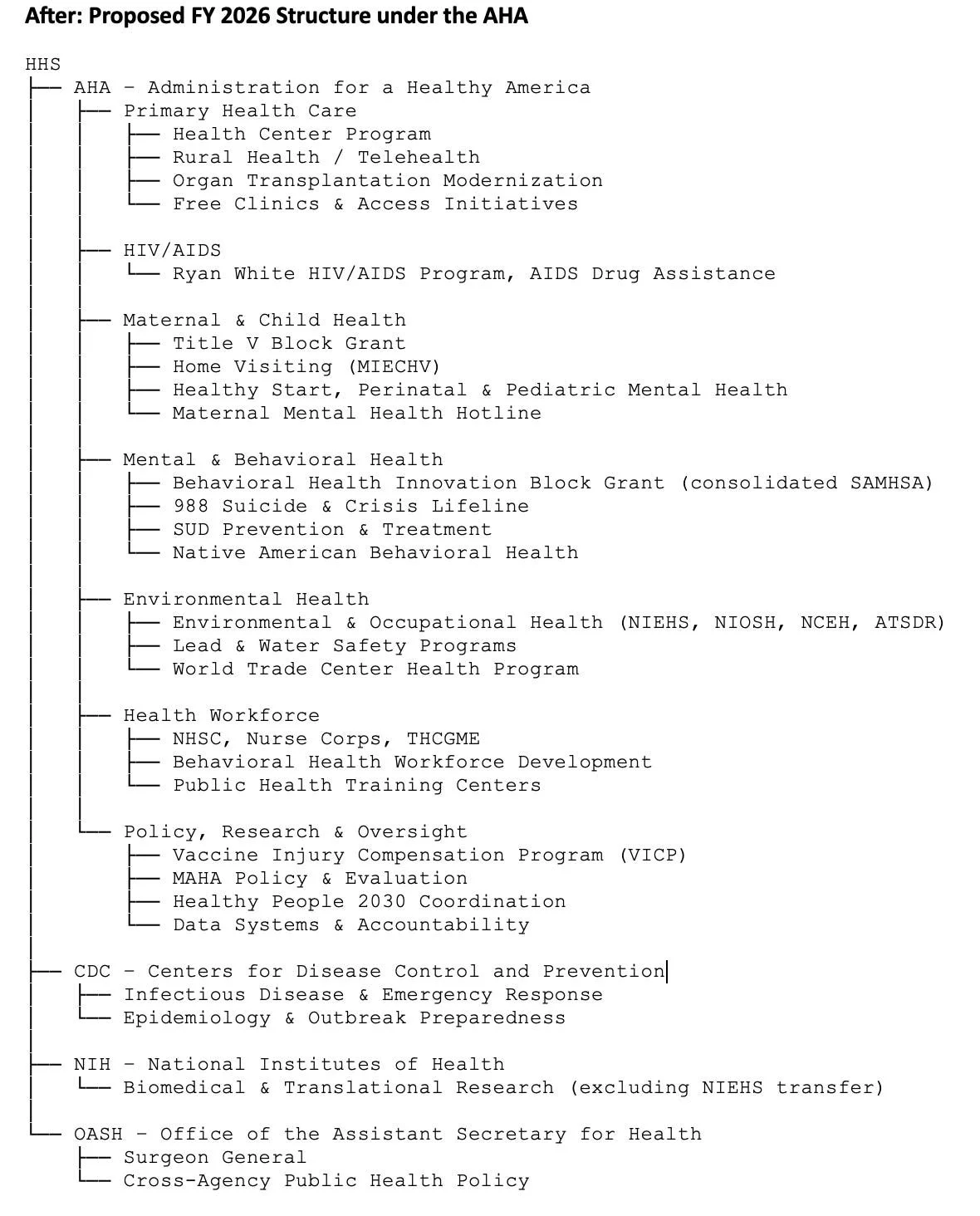
The initiatives and programs that will be consolidated from other agencies and institutes under AHA is what make this proposal significant.
The AHA represents one of the most sweeping reorganizations within the Department of Health and Human Services (HHS) since its formation, essentially merging programs that were scattered across multiple operating divisions (OPDIVs) into a single agency focused on public health, prevention, environmental health, and the health workforce.
Here’s a detailed breakdown of which agencies and programs would be consolidated into the new AHA, based on the FY 2026 AHA Congressional Justification (CJ) and HHS’s FY 2026 Budget Overview:
1. Origin and Purpose
AHA is described as a new operating division (OPDIV) within HHS.
It is designed to “bring together functions currently spread across multiple OPDIVs” to strengthen coordination and reduce duplication in:
Primary care & health centers
Mental & behavioral health
Environmental health & safety
HIV/AIDS services
Maternal & child health
Health workforce programs
2. Major HHS Components Being Moved into AHA
👉 In short, nearly all of HRSA’s programmatic components except grant administration and certain policy functions move to AHA.
→ Essentially, SAMHSA ceases to exist as a standalone OPDIV; its functions are integrated into AHA.
This transfer makes AHA the home for all environmental and occupational health functions formerly split between NIH, CDC, and HRSA.
Note: The Surgeon General of the United States is the operational head of the U.S. Public Health Service Commissioned Corps (USPHS). It is organizationally housed under the Office of the Assistant Secretary for Health (OASH) within HHS and will not be moved to AHA. The Surgeon General’s direct supervisor is the Assistant Secretary for Health (ASH).
So CDC keeps communicable disease and epidemiology; AHA takes over chronic disease prevention and environmental exposures.
3. Newly Created or Reorganized AHA Accounts
AHA’s structure combines all these transferred programs into seven major budget accounts:
Primary Health Care
HIV/AIDS
Maternal and Child Health
Mental and Behavioral Health
Environmental Health
Health Workforce
Policy, Research, and Oversight
Each account consolidates multiple legacy programs from HRSA, SAMHSA, OASH, CDC, and NIEHS.
4. What’s Eliminated or Absorbed
The CJ explicitly lists:
23 programs eliminated from Primary Health (mostly HRSA small earmarks and categorical grants)
9 programs eliminated from Environmental Health (mostly overlapping research initiatives)
40 programs eliminated from Mental Health (SAMHSA legacy discretionary grants)
14 programs eliminated from Health Workforce (small categorical training programs)
The goal, per the CJ, is “reducing duplication and redirecting funds toward streamlined block grants and large-scale initiatives.”
5. Strategic Intent
Create a single “home for prevention and wellness” inside HHS.
Integrate behavioral, environmental, and primary health under one management chain.
Simplify state/federal funding streams (especially block grants).
Improve coordination between chronic disease prevention, workforce policy, and data systems.
Enable cross-cutting evaluation and accountability for outcomes instead of dozens of fragmented program metrics.
Below are charts showing which agencies shrink or disappear under the AHA plan.
Summary of Changes
• Substance Abuse and Mental Health Services Administration (SAMHSA) eliminated as a standalone operating division; all functions moved to the AHA
• Health Resources and Services Administration (HRSA) programs (except for small administrative and policy offices) absorbed into the AHA
• National Institute of Environmental Health Sciences (NIEHS) environmental health portfolio moved from the National Institutes of Health (NIH) to the AHA
• Centers for Disease Control and Prevention (CDC) environmental and occupational health programs — including the National Center for Environmental Health (NCEH), the Agency for Toxic Substances and Disease Registry (ATSDR), and parts of the National Institute for Occupational Safety and Health (NIOSH) — transferred to the AHA
• Office of the Assistant Secretary for Health (OASH) programs such as the Vaccine Injury Compensation Program (VICP) and Healthy People 2030 coordination shifted to the AHA.*
In Summary
The creation of the Administration for a Healthy America (AHA) represents a forward-looking transformation within the U.S. Department of Health and Human Services. By bringing together key programs and expertise from several long-standing agencies, AHA is designed to deliver a more integrated and efficient approach to improving the nation’s health. Its central mission is to unify prevention, behavioral health, environmental safety, and workforce development under one coordinated structure, helping Americans live healthier lives while strengthening the public health system.
This realignment draws together the strengths of the Health Resources and Services Administration, Substance Abuse and Mental Health Services Administration, and major environmental health functions from the National Institutes of Health and the Centers for Disease Control and Prevention. It also incorporates important public health coordination activities from the Office of the Assistant Secretary for Health. By aligning these programs under one organizational umbrella, the AHA can streamline grant administration, reduce duplication, and focus on measurable outcomes in primary care, mental health, maternal and child health, environmental health, and workforce capacity.
The consolidation is also expected to streamline operations and save money for taxpayers by eliminating overlapping administrative layers and combining similar grant and support programs into unified funding structures. This means fewer redundancies, simplified reporting, and shared data systems, thus allowing federal resources to be used more effectively and ensuring that more funding reaches communities directly. In the long run, these efficiencies will strengthen accountability and transparency while reducing overall costs associated with managing multiple separate agencies.
The new structure builds a stronger bridge between science, policy, and community impact. It places equal emphasis on prevention and access, ensuring that health services, research, and workforce development are coordinated to meet people where they are: particularly in rural and underserved communities. Through this integration, HHS aims to modernize public health delivery, improve accountability, and strengthen the nation’s ability to prevent illness rather than merely respond to it. The AHA thus stands as a cornerstone for a healthier, more equitable, and more resilient America.
All that said, organizational change is hard, and this reorganization is on a scale not attempted by the US government in decades.
Executive action alone cannot achieve this transformation; it must be supported by Congressional legislation and long-term budget commitments. The Senate Appropriations Committee’s budget report from July, 2025, does not specify a clear appropriation line for AHA. The language in the report related to the drafts does not seem to endorse the full reorganization plan of AHA (which involves consolidating multiple agencies and functions) in statutory form.
Congress appears to be waiting or undecided on whether to adopt the proposed AHA structure. Without statutory authorization of AHA, funds remain under legacy agencies.
“Establishing the Administration for a Healthy America”
Finally, an act of Congress must formally create the Administration for a Healthy America (AHA) to birth it into permanent existence. So far, Congress has not yet introduced or passed legislation that specifically authorizes AHA as a distinct agency under the law.
If AHA is to become fully operational and fully funded under its own budget account, future legislation and appropriations language will likely need to explicitly authorize it and create the appropriation line for it.
We call on Congress to work together on this critical reorganization of HHS. The time is now to act.