Vaccines and Adjuvants: Aluminum
Just the facts, M'aam.
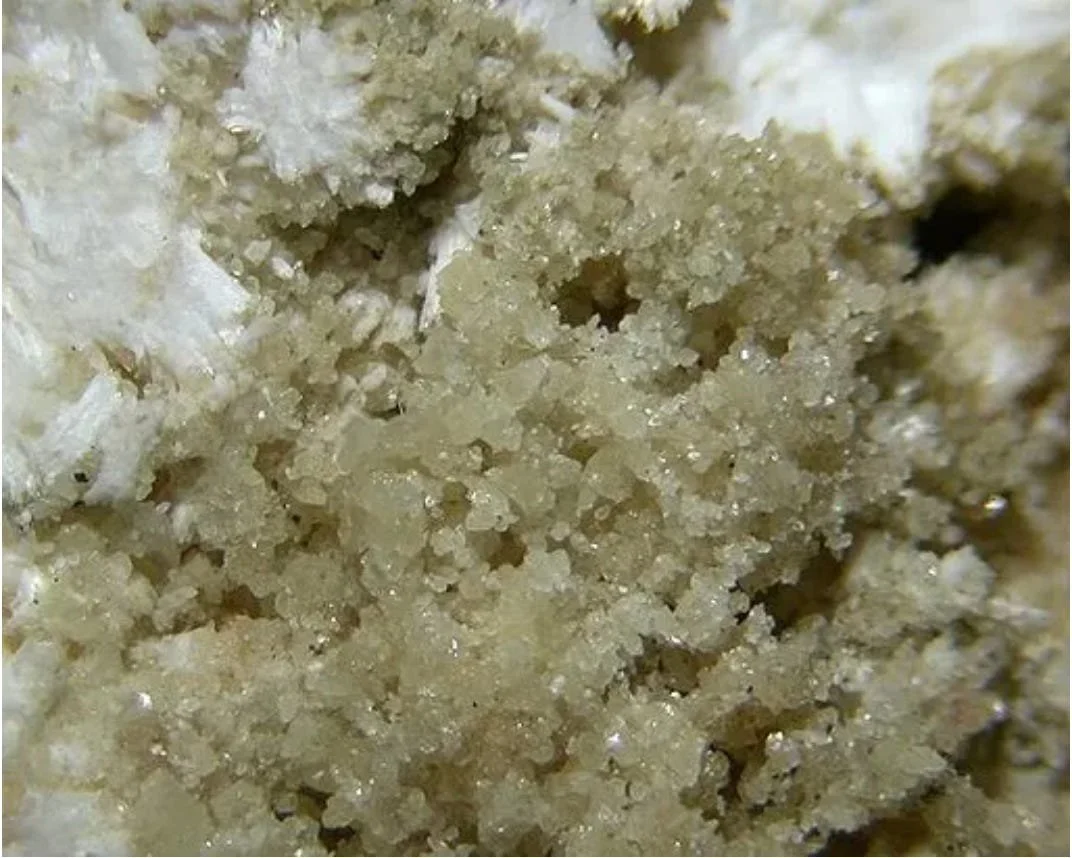
Image of Bohmite, the mineral version of the common Aluminum vaccine adjuvant known as Alum. Chemically, the crystalline aluminum oxyhydroxide AIOOH. The structure consists of corrugated sheets of aluminum octahedra.
Are all vaccines similar, and what ingredients are in vaccines?
Each approved vaccine is a unique mixture of both ingredients and manufacturing processes. From a regulatory standpoint, vaccine products are a combination of ingredients, manufacturing process, process controls (including release testing), and supporting safety and efficacy/effectiveness testing. The repeated assertion that all vaccines are safe and effective is mere propaganda. Each licensed vaccine product has its own profile of risks, benefits, pharmacology, immunology, and other characteristics. In general, a vaccine “final drug product” consists of antigens, adjuvants, preservatives (in many cases), stabilizers and other “excipients”, surfactants, residuals (eg permitted contaminants), a diluent, and in some cases adulterants (contaminants at levels that are not permitted).
Preservatives are included in multi-dose vials to prevent bacterial or fungal contamination after the vial is opened. The most commonly used preservative is 2-phenoxyethanol, while thimerosal (containing ethylmercury) was historically used but is no longer present in most routinely used vaccines in the U.S.
Stabilizers protect the vaccine during manufacturing, storage, and transport by preventing chemical degradation and preventing components from sticking to the vial. Common stabilizers include sugars (like sucrose or lactose), amino acids (such as glycine), gelatin, and proteins like recombinant human albumin.
Surfactants are used to keep all ingredients evenly mixed in the liquid formulation, preventing clumping or settling. These are also found in some foods, such as ice cream.
Residuals are trace amounts of substances left over from the manufacturing process, such as egg proteins (from egg-based production), yeast, antibiotics (like neomycin or polymyxin B), or formaldehyde used to inactivate pathogens.
Diluents, typically sterile water or saline, are used to reconstitute freeze-dried vaccines or adjust the concentration before administration.
For the sake of discussion, vaccine products can be divided into three general categories.
1. Live Vaccines
Classically, “live” vaccines are essentially replication-competent viruses, bacteria, or potentially other replication-competent biological material. Simple examples include the oral polio vaccine, the yellow fever vaccine, the smallpox vaccine, and the Tuberculosis vaccine (BCG). A more recent example of this category is the “Flumist” influenza virus vaccine. In all of these cases, the patient is offered a product that actually infects them in some way, but - assuming that they have a “normal” properly functioning immune system - will not cause clinical disease. If the patient is immunosuppressed in some way, all bets are off. In the case of “live” vaccines, dosage, purity, identity, and “titer” of the product are critical. To illustrate this with a simple example, if you take multiple doses of yellow fever vaccine in close succession, you will get clinical yellow fever, and it can kill you. In general, “live” vaccines are the most effective, as they most closely mimic actual infection by a pathogen. However, they do cause the cells and tissues of your body to actually manufacture foreign proteins, similar to gene therapy-based vaccines.
2. Dead Vaccines.
“Dead” vaccines were originally prepared by taking a “live” replication-competent agent (virus or bacteria), growing it in some sort of material that will support replication (fermentation broth, cell culture, or fertile/embryonated chicken eggs for example) and “killing” or inactivating it in some way, typically by adding a chemical that would either break up the agent into its components, or damage its genome so that it could no longer replicate. One major problem with these types of products is purity, as this category is prone to contamination coming from the material used to support replication of the pathogen. The early anthrax vaccines used by the US Military during “Desert Storm” were notoriously “dirty” or contaminated with material that had nothing to do with the parts of the killed anthrax that were intended to be included in the product. Over time, various methods have been developed to produce much purer “antigens” or immunogenic components (including the use of recombinant DNA together with fermentation and advanced purification technology), but the paradox has been that as the preparations became purer, their “immunogenicity” was reduced. Essentially, the impurities were biologically active and often increased the adaptive (and innate) immune response to the intended “antigen” from the pathogen. This relates to the topic at hand, that being the use of “adjuvants” in vaccines. A related point is that, in the case of modern “subunit” vaccines produced using recombinant DNA technology, the biologically active “antigen” is produced outside your body and then injected. This is very different from the next and newest category of vaccines and technologies.
3. Gene Therapy-based Vaccines
The newest (third) category involves the use of recombinant DNA and/or gene therapy technologies to cause your body to manufacture some part of a pathogen, which, when presented to your immune system by your own cells, causes your body to mount an immune response (innate and/or adaptive) to the foreign protein derived from a pathogen. In many ways, this is similar to the first category, live attenuated vaccines. In the case of live attenuated vaccines, a weakened version of the pathogen is injected (or swallowed) and it replicates in your body. In the case of gene therapy-based vaccines, either a recombinant virus (such as an adenovirus) or a non-viral gene delivery formulation (mod mRNA or DNA) is administered, and this causes your body to produce a part of the pathogen (such as the spike protein from SARS-CoV-2). Another variant of this involves engineering the vesiculovirus (VSV) to display an Ebola virus protein on its surface - this is the Merck VSV Ebola vaccine. In that case, the VSV acts both as a gene therapy vector producing a specific adaptive immune response to Ebola, and also triggers a strong innate immune response. Up for discussion in that case is which is the more important active component. The latest version of gene therapy tech used for vaccination involves self-replicating RNA vectors based on alphaviruses.
In the case of the lipid nanoparticle-delivered mod mRNA vaccines, the inclusion of small DNA fragments derived from the bacterial DNA used to make the mod mRNA is probably a form of an adjuvant, much like other adjuvants commonly used with “killed” vaccines.
Adjuvants and Vaccines
What is an adjuvant? Quite simply, a vaccine adjuvant is any substance or compound added to a vaccine to enhance the body’s immune response to the antigen (the part of the vaccine that mimics the pathogen). This broad definition underscores the “anything goes” nature of adjuvants. You can find a pretty comprehensive list of known adjuvants here. This list was compiled by vaccine experts from both DoD and NIH/NIAID who were friends of mine, back in the days when I was very involved in AIDS vaccine development. It used to be available for download on the NIH website, but has since been removed. Fortunately, I kept a copy and have now made it available for downloading. It is a bit dated, but still represents the most comprehensive summary of adjuvants that I am aware of.
Adjuvants are used by researchers and the vaccine industry to stimulate adaptive immune responses to pathogen-specific antigens. At a simplistic level, you can think of an adjuvant as something that provides a “danger signal” to the immune system, causing it to respond to a foreign molecule when it otherwise might not respond. Typical adjuvants act to increase the strength and duration of the immune response, allow lower doses of antigen to be effective (dose-sparing), broaden the immune response (e.g., against drifting viral strains), direct the type of immune response (e.g., favor antibody production or T-cell activation), and improve overall vaccine efficacy in populations with weaker responses (infants, elderly, immunocompromised).
As discussed above regarding the category of “dead” vaccines, industry experience has been that, in general, the more pure the vaccine antigen, the less active it is for eliciting a robust adaptive (B and T cell) immune response. In other words, An adjuvant is an immune-response “booster” deliberately included in some vaccines to make them work better.
Note that the FDA does not “license” adjuvants. What are licensed are vaccines that are formulated with various adjuvants.
General categories of adjuvants include the following:
Aluminum salts (alum) – oldest (1920s) and most widely used (in many childhood vaccines like DTaP, hepatitis B).
Oil-in-water emulsions – e.g., MF59 (in some flu vaccines for elderly), AS03 (in pandemic flu vaccines)
Liposome-based – e.g., AS01 (in Shingrix shingles vaccine and some malaria vaccines)
TLR agonists – e.g., CpG 1018 (in Heplisav-B hepatitis B vaccine), MPL (in Shingrix)
Saponin-based – e.g., QS-21 (in Shingrix and some COVID/malaria vaccines)
Aluminum Adjuvants and Vaccines
Various forms and formulations of aluminum salts are used as vaccine adjuvants. These preparations are among the oldest and most widely used adjuvants. These are NOT the same as powdered metallic aluminum or free aluminum ions, which ARE highly toxic to humans.
Almost every inactivated or subunit vaccine given to infants and young children contains aluminum (except pneumococcal conjugates and Hib PedvaxHIB).
Aluminum-based adjuvants tend to bias immune response to the co-administered antigen towards antibody production, and away from adaptive cellular (effector T cell) responses. Most viruses and intracellular pathogens are predominantly controlled by a combination of innate and adaptive cellular immunity. A case can be made that, in this context, antibodies mostly function as a mechanism to clear up viral fragments and debris.
Many novel or experimental adjuvants employ aluminum salts together with other agents (liposomes etc.)
Most live vaccines and modern conjugate/mod mRNA vaccines do not contain aluminum.
Clinical Syndromes associated with aluminum powder, aluminum ion or injected aluminum exposure toxicity include
Dialysis encephalopathy (dialytic dementia)
Caused by high aluminum in dialysis fluid pre-1980s
Symptoms: speech disturbance, seizures, myoclonus, psychosis
Now extremely rare due to water treatment standards
Parenteral Neonatal (PN) Aluminum Toxicity
Preterm infants exposed to 4–5 μg/kg/day IV aluminum via parenteral nutrition show neurodevelopmental and bone toxicity.
These findings led to FDA aluminum limits for parenteral nutrition solutions.
Vaccine-day aluminum doses, although differing in chemical structure from free aluminum ions, can be orders of magnitude higher per kg than PN limits.
Aluminum-induced bone disease (osteomalacia)
Seen in long-term parenteral nutrition or dialysis patients
Fracturing bone pain, hypercalcemia, resistance to vitamin D
Pulmonary fibrosis / aluminosis
From chronic intense inhalation of aluminum powder
Rare occupational disease
Macrophagic myofasciitis (MMF)
Persistent aluminum-containing granulomas at intramuscular injection sites (mostly deltoid)
Symptoms in many MMF patients: chronic myalgias, fatigue, and cognitive difficulties.
Detected in some patients with myalgia, fatigue, and cognitive issues
Causal link to systemic symptoms is not universally accepted
Muscle biopsies show aluminum-loaded macrophages (MMF lesions) at prior vaccine sites years later. This demonstrates long-term persistence of aluminum adjuvants in human tissue.
Examples of Aluminum salt vaccine adjuvants (from the Vogel et al Adjuvant Compendium)
Note that none of these are elemental or ionic free aluminum forms, but rather comprise various aggregate or semi-crystalline forms of aluminum. Therefore, information involving pharmacodynamics, pharmacokinetics, pharmacodistribution, general toxicology, and pathology developed using exposure to elemental or ionic forms of aluminum are unlikely to be fully predictive for these alternative forms and formulations of aluminum.
“Alum”, a common aluminum adjuvant formulation, does not refer to crystalline aluminum oxyhydroxide (AlOOH); true alum is a double sulfate salt such as potassium alum, KAl(SO₄)₂·12H₂O.
Current Aluminum salts used in most licensed human vaccines are not Alum, but rather consist of:
AH (aluminum oxyhydroxide gel)
AP (aluminum hydroxyphosphate)
AAHS (amorphous aluminum hydroxyphosphate sulfate) (Merck property)
Summary of Aluminum-containing vaccines
The following is a comprehensive list of commonly used vaccines that contain aluminum salt adjuvants (aluminum hydroxide, aluminum phosphate, or potassium aluminum sulfate/alum) as of 2025.
Routine Childhood/Adolescent Vaccines (Containing Aluminum). Almost all non-live vaccines for infants/children use aluminum adjuvants.
Adult and Travel Vaccines (Containing Aluminum)
Abbreviated Risk Analysis, Aluminum in Vaccines
Federal Aluminum Regulatory Limits: The U.S. Code of Federal Regulations (21 CFR 610.15(a)) limits aluminum in vaccines to ≤0.85 mg per dose, regardless of age group.
The limit of 0.85 mg per dose is not derived from pharmacokinetic and safety studies, but was first proposed in the 1960s, based on 1947 and 1952 short studies in solution containing potassium alum (please see Angrand et al., 2025).
The Agency for Toxic Substances and Disease Registry (ATSDR) is a federal public health agency within the U.S. Department of Health and Human Services (HHS). ASTDR has assessed and determined a “minimum risk level” (MRL, somewhat akin to NOAEL determination typically used by FDA) for orally ingested aluminum (very low absorption), which cannot be considered equivalent to injected forms. ATSDR: oral minimal risk level ≈ 1 mg (1,000 μg) Al/kg/day based on animal data. This assumes only ~0.1% oral absorption. Converted to an injected-equivalent threshold, this approximates 1 μg/kg/day.
This limit was then tested in the rabbit study (Flarend et al., 1997). The observation was: retention of 94% & 78% of injected ABAs AND cerebral translocation. No other signs of toxicity were observed, because such “acute or chronic adverse effects” were not questionned in this paper (see Masson et al., 2018). These findings are not consistent with this being a NOAEL dose.
Although the FDA imposes individual dose limits on vaccine-associated aluminum during licensure, it does not provide oversight or guidance on concurrent or proximal administration of multiple aluminum-containing vaccines. This issue is illustrated in the following graphic:
Biodistribution and Pharmacokinetics
In the only published/peer-reviewed study of aluminum ion blood levels observed in infants after aluminum-adjuvant containing vaccine administration (Movsas et al. (2013), serum aluminum levels measured before and 24 hours after vaccination showed no significant mean increase. This exploratory study is associated with significant limitations, including very small sample size (n= 15), only 24-hour follow-up, and no organ or long-term distribution data.
Experimental and clinical data suggest IM aluminum can persist at the injection site, then migrate via immune cells to liver, spleen, and brain. Exley and colleagues have demonstrated that aluminum is detectable in most human brains, reflecting cumulative environmental exposure. Very high aluminum levels have been reported in brains from individuals with autism, AD, MS, and other conditions. In autism studies, aluminum in the brain is often localized within microglia and other inflammatory cells.
Toxicology Data Gaps and Ambiguity
Currently available infant safety assessments rely on a small number of toxicokinetic studies and modeled assumptions.
No long-term human studies tracking vaccine-derived aluminum kinetics in infants or children have been published.
Critical reviews highlight errors in absorption factors and clearance assumptions in influential models (e.g., Mitkus 2011). Modeling-based correction for these assumptions markedly increases modeled body burden relative to toxicity thresholds.
No large, prospective, well-controlled studies comparing neurodevelopmental or autoimmune outcomes by cumulative aluminum dose have been performed or published.
No established safe dose of injected aluminum for neonates and preterm infants has been established.
Existing toxicology and PK data are too sparse and model-dependent to support definitive conclusions of safety at current cumulative doses.
In Conclusion:
This peer-reviewed paper nicely summarizes the situation regarding the use of Aluminum vaccine adjuvants. Little has changed since its publication in 2011.
Aluminum vaccine adjuvants: are they safe?
Curr Med Chem 2011;18(17):2630-7. L Tomljenovic, C A Shaw
Neural Dynamics Research Group, Department of Ophthalmology and Visual Sciences, University of British Columbia, Vancouver, BC, V5Z 1L8, Canada.
Abstract
Aluminum is an experimentally demonstrated neurotoxin and the most commonly used vaccine adjuvant. Despite almost 90 years of widespread use of aluminum adjuvants, medical science’s understanding about their mechanisms of action is still remarkably poor. There is also a concerning scarcity of data on toxicology and pharmacokinetics of these compounds. In spite of this, the notion that aluminum in vaccines is safe appears to be widely accepted. Experimental research, however, clearly shows that aluminum adjuvants have a potential to induce serious immunological disorders in humans. In particular, aluminum in adjuvant form carries a risk for autoimmunity, long-term brain inflammation and associated neurological complications and may thus have profound and widespread adverse health consequences. In our opinion, the possibility that vaccine benefits may have been overrated and the risk of potential adverse effects underestimated, has not been rigorously evaluated in the medical and scientific community.
It is time for a re-assessment of this widely used vaccine adjuvant, given the many questions about its adverse effects and toxicity…